Supportive care you can offer during fever
Often, we only hear: Do not reduce the fever! That's true, but what can we do then?
We do not have to idly wait before making ourselves useful.
Management principles in four main points:
- Monitor the course of the fever.
- Provide the right amount of fluid and nutrition.
- Calm down and focus on taking care of your child. Nurture your relationship, lend emotional support.
- Carefully monitor symptoms and reasonably assess the risk of the situation.
1) Monitoring the fever
This means that we are not preventing the body from doing what it is doing (because it is actively fighting the illness) but instead supporting the warmth process.
The elevated temperature does not need to treated or eliminated, but we can soothe its unpleasant consequences. Thesesteps are described in detail in the section titled “Methods for fever reduction”.
2) Fluid and energy intake
Each 1°C rise in temperature increases metabolism by 10% and fluid requirements by 12%.
This results in a negative energy balance due to increased energy use (catabolism) and loss of appetite (which is physiologically normal).
Sweating, aswell as increased metabolic processes also cause loss of fluid and electrolytes (salts).
Liquid: make sure that the child drinks regularly by taking sips. The problem is that children are often reluctant to drink, so they need to be reminded to do this.
It often helps to give them a sip of a warm, pleasant liquid that they request or accept from a spoon. Basically all liquids are suitable (but preferably not cow’s milk, or sugary or carbonated drinks). Herb and fruit teas, with a little honey; diluted juices, and mineral water are best.
The following teas have traditionally proved their worth:
- in the case of fever linden blossom, elder flower
- chamomile for abdominal pain
- sage for sore throat
- lavender, lemongrass in the case of restlessness
- Breastfeeding is best for breastfed infants. If the child spits up or vomits, you can try a small amount of feeding again after a short break.
If fever is accompanied by vomiting and diarrhea, give the patient an oral rehydration solution (ORS). The taste will be milder, when the fluid is cool. If a child will not sip it from a glass, it can be given the fluid with a straw, a spoon or syringe, a few millilitres at a time. ORS contains a sufficient amount of minerals (sodium, potassium, chlorine, citrate) and sugar (glucose).
Nutrition: It is not a problem if your child's appetite is poor for a few days.
We recommend a low-fat, high-carbohydrate diet taken as individual bites, as much as your child requests.
Rice, millet, bite size pieces of steamed vegetables, fruits. Preferably in the morning when the fever is lower.
Children typically regain any lost kilograms quickly after the fever has passed and gain even more strength.
3) Keeping calm and connected = providing comfort
For more complete healing, special care should be taken to ensure a calm and peaceful atmosphere around the patient. It should be free of electronic devices (TV, computer, smartphone, etc.). Because those devices capture childrens attention, they are only seemingly relaxing. In reality the flood of information they are taking in all needs to be processed, which means additional internal work.
Feverish children should not enter the community, they should not be out in public. They shouldn't strain themselves either physically or intellectually. Reduce social stress. Stay at home with the child, provide a calm atmosphere. The child doesn't have to stay in bed all the time.
The rooms should be well ventilated.
Many consider feverish conditions provide an opportunity to develop a loving and supportive relationship (78-81). It’s "a little break" from the often too busy pace of everyday life. The febrile period is a "special occasion" during which it is worth engaging more intimately with your child.
External interventions such as compresses, rubs, oil wraps, foot baths, etc. - applied properly and in the right context - are especially nice opportunities to non-verbal care for and communicate with your child. See our article on antipyretic methods for more instructions. Natural medicinal preparations may be administered as required (e.g. herbal teas, herbal extracts).
In a study with Harvard medical students, the students experienced a positive change in their relationship toward the disease when they were cared for in a calm atmosphere during their feverish condition.
Sometimes, for example, autistic children are strikingly more communicative and empathetic during fever (99, 100).
4) Monitoring the symptoms (risk assessment)
For more details see our articles "How dangerous is fever" and "Accompanying symptoms of fever".
By observing some phenomena, a distinction can be drawn between harmless and more serious states.
- Skin rash and skin colour
- Activity, consciousness
- Respiratory rate
- Heart rate
- Hydration
- Other
Signs of dehydration:

For the little ones inculde: a dry mouth, plaque on the tongue, lack of tears, sunken eyes, the large fontanelle is sunken as compared to the bones around it (fontanelle: the little round "softness" on top of the baby's head), less urine, decreased firmness of the skin.
For older children: fatigue, dizziness, headache, rapid heartbeat, nausea, muscle cramps, decreased consciousness.
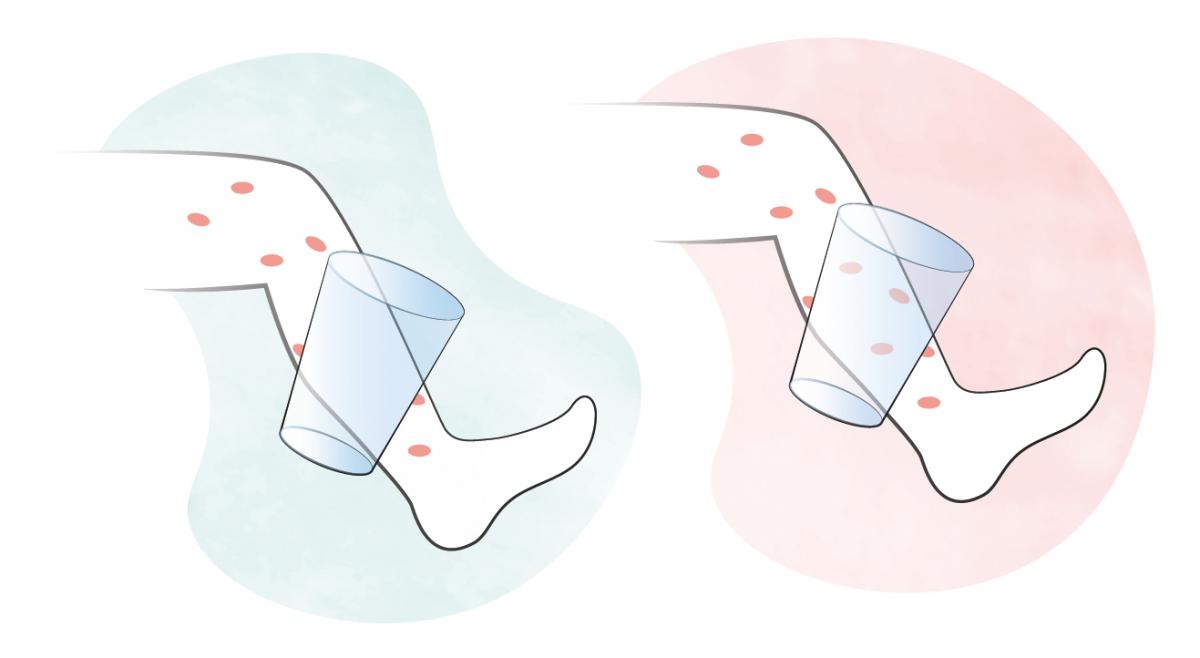
How to distinguish harmless skin rashes from dangerous purpuric rashes (petechiae) on a child's body with a glass test?
Gently press the side of a drinking glass onto the area of skin in question - if the skin does not blanch (meaning, the redness goes away) when you are gently pressing down with the glass it is most likely a purpuric rash - if you notice such, consult a doctor immediately!
The rash on the left is not dangerous because it can be suppressed (blanching).
The red rash on the right is purpuric (non-blanching) rash and it's dangerous.
According to the professional protocol:
- Make the child drink regularly (breastfeeding is best for breast-fed infants) to avoid loss of fluid and dehydration.
- Look out for signs of dehydration (such as dry mouth, plaque on the tongue, lack of tears, closed eyes, sunken large fontanelle (fontanelle: little round "softness" at the top of the baby's head that closes around 1.5 years), less urine.
- Encourage your child to continue drinking if signs of dehydration occur.
- A patient with fever should not be out in public.
- Do not under- or over-dress children.
- Do not use cold baths, cold sheets.
- Make all interventions a pleasant experience
- If the cause of the fever is unknown, antibiotics should not be given. Antibiotics should only be prescribed by a physician.
You can find the corresponding numbered references here: References
Version update: 1 March 2024